 Each and every state has a Medicaid program. Some states offer a wider range of programs within their Medicaid system than others do. In New Mexico, there are approximately 40 categories of eligibility. According to the state’s website, New Mexico’s Medicaid program serves 1 in 3.
Each and every state has a Medicaid program. Some states offer a wider range of programs within their Medicaid system than others do. In New Mexico, there are approximately 40 categories of eligibility. According to the state’s website, New Mexico’s Medicaid program serves 1 in 3.
Medicaid is a public, or government run, form of health insurance. It is designed to provide affordable health insurance coverage for people who are low-income and who cannot afford to purchase health insurance coverage from a private company. Medicaid funding comes from both the federal government and from the government of an individual state.
In New Mexico, the Medicaid program is administered by the New Mexico Human Services Department. More specifically, it is run by the Human Services Department’s Medical Assistance Division (MAD). Right now, New Mexico has about 40 categories of eligibility within the state’s Medicaid program. Each is designed to cover a certain population, (such as children, teens, pregnant women, cancer patients, people who are disabled, and more).
One of the programs is called “Insure New Mexico! Solutions”. To be eligible for this program, a person must be a resident of New Mexico, and must also be a United States citizen or permanent legal resident. Legal permanent residents must be able to show original documentation from INS that indicates immigrant status and date of legal entry. Legal immigrants must have been a qualified alien for five years before they can be eligible for Medicaid.
This program is for low-income, working adults, who have countable household income up to 200% of the federal poverty level. The person must be between the ages of 19 and 64. The person must have no current health insurance coverage, and must not be eligible for certain government health insurance benefits.
People who have had a voluntary cancellation of health insurance coverage in the last six months will not be eligible for Medicaid. According to the website:
“It is not considered a voluntary cancellation when an individual or spouse fails to take advantage of an offer of health insurance by an employer, or fails or refuses to take advantage of COBRA continuation policy. Also not considered voluntary cancellations are loss of access to employer-sponsored insurance due to loss of employment, divorce, death of a spouse, geographic move, loss of coverage as a dependent child, or loss of Medicaid eligibility due to ineligibility.”
My understanding of this is that “voluntary cancellation” means that you were able to afford to buy a health plan from a private company, so you did. But, later, you decided to cancel this plan in an effort to qualify for Medicaid, instead.
There are no pre-existing condition limitations for Medicaid eligibility. There also is no asset test required for eligibility.
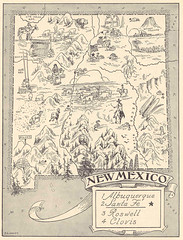
Image by Meta Mourphic on Flickr

